Why Have I Got Blood Vessels Growing In My Eye?
It is not uncommon to be told during a contact lens check-up at your Opticians, that you have 'blood vessels' growing in your eye, caused by excessive contact lens wear. It is a condition called corneal vascularisation.
Despite its prevalence in the contact lens community, chances are you’ve never heard of corneal neovascularisation (CNV). Unfortunately, the first time most contacts-wearers learn about CNV is after they’ve been diagnosed with the condition by their Optometrist. Left untreated, CNV could have disastrous effects on your vision. So, if you wear contact lenses every day, it’s a good idea to learn the warning signs of CNV to be proactive about your eye health.
In this post, we’ll teach you everything you need to know about this potentially blinding disorder. After going over exactly what CNV is, we’ll share a few potential treatment strategies and preventative measures you could discuss with your Optometrist.
What Is Corneal Neovascularisation?
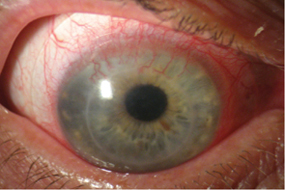
Corneal vascularisation is the growth of new blood vessels in the eye, more specifically on the cornea, this is caused by a lack of oxygen reaching the cornea and if untreated can be sight threatening.
The scientific name for oxygen deprivation in the cornea is known as corneal hypoxia and, if this occurs regularly enough or long enough then it can result in various severities of Cornel vascularisation.
This condition has been known to Optometrists since the 1920's, when it was first noted in the wearers of large solid contact lenses called scleral lenses. Today it is still a potential problem for soft contact lens wearers.
Since contact lenses cover the corneas, oxygen reaching the cornea is reduced, even with high water content lenses or silicone lenses with over wear oxygen deprivation can occur.
When deprived of oxygen the cornea starts to swell, they then try to pull nutrients from surrounding structures, which results in new blood vessel growth.
If your eyes are often red when you wear contact lenses, it’s a clear warning sign your eyes are in distress. Without prompt treatment, CNV could gradually develop and these new blood vessels if unchecked and treated can lead to sight be sight threatening.
In the fight against Corneal vascularisation, it is important not to overwear contact lenses and to attend contact lens checkups regularly.
What Causes Corneal Neovascularisation?
The greatest risk factor for developing CNV is wearing contact lenses for extended periods of time - and especially sleeping overnight in contact lenses that are not designed for this purpose. No matter how long your contact lenses are approved for use, it’s always a good idea to take them out once in a while to give your eyes a breather (literally). You should always throw away lenses as soon as they’ve passed their expiration date to avoid CNV and other eye conditions.
Other factors that predispose towards this complication include using dirty or degraded lenses or low water content lenses - especially thick ones and tight lenses that trap debris.
It’s especially important to take out your lenses before going to sleep every night. Closing your eyelids for extended periods of time will reduce the amount of oxygen reaching your eyes, add to this a barrier caused by contact lens wear and you have the potential to seriously reduce the amount of oxygen reaching your eye whilst you sleep.
Contact lens wearers who frequently wear their lenses at night significantly increase their risk of developing Corneal neovascularisation.
The only contact lenses approved for overnight wear are ortho-k gas permeable lenses and continuous or extended-wear contact lenses. All other contact lenses need to be removed before bedtime.
One study reported an estimated incidence rate of 1.4 million people per year, 12% of whom suffered subsequent loss.
Although a lack of oxygen is the primary cause of CNV according to the Columbia University Department of Ophthalmology these can include infection, trauma, chemical burns, immunologic diseases, degeneration or intraocular events such as uveitis, glaucoma and phthisis bulbi.
What Are The Signs Of Corneal Neovascularisation?
A major problem with Corneal neovascularisation is that it usually presents no obvious warning signs.
The most obvious sign of Corneal neovascularisation is red blood vessels on the whites of your eye these can sometimes be visible in the iris too, you may also experience some or all of the symptoms below
- Redness around the cornea.
- Pain.
- Light sensitivity.
- Decreased vision or blurring.
- Pain when wearing contact lenses or being able to wear them for shorter periods of time.
- Tearing.
While you might experience some eye discomfort and light sensitivity, the warning signs aren’t generally severe and could easily be brushed off as dry eye syndrome. Even if you see the red blood vessels protruding around your eyes, you might mistakenly think your eyes are just bloodshot due to stress or a late night out.
Since Corneal neovascularisation is so hard to detect in the early stages, it’s crucial for contact lens wearers to see their optometrist at least once per year for vision checkups. Only an eye specialist can detect the early warning signs of CNV and put you on an actionable treatment plan.
Treatment for Corneal Neovascularisation
The treatment for Corneal neovascularisation will depend on the cause of the condition, if like many cases it is due to contact lens wear then the first step is to stop wearing contact lenses, this may not need to be a permanent cessation but rather a hiatus, once your eye recover then your Optometrist may discuss other contact lens options with you.
The American Academy of Ophthalmology (AAO) has suggested the use of anti-inflammatory medication, monoclonal anti-VEGF antibodies and MMP inhibitors have shown promising results and should all be explored fully before considering invasive surgical options.
Over time, the vessels can drain blood and become what is known as 'ghost vessels'. Over several years even these can regress and clear. The condition will need careful management by your Optometrist.
How To Prevent Corneal Neovascularization
It is important to protect your eyes, whether outside in the sun, whilst using chemicals or undertaking dangerous tasks and whilst wearing contact lenses.
We advise wearing good quality sunglasses that protect against UVA and UVB rays and industry-approved safety goggles when performing dangerous working tasks that could lead to eye injury.
If you are a contact lens wearer, do not sleep in your contact lenses, only wear them as directed by your Optometrist, clean and store lenses as directed and attend regular checkups.
If you have a bad habit of keeping your contact lenses on while you nap or sleep, don't be afraid to raise this with your Optometrist, he or she can recommend the best lenses for you, this could be a silicone lens such as 1 Day Acuvue Trueye, which will discourage hypoxic (low oxygen) conditions from arising and so prevent any further vascularization1 Day Acuvue Trueye allows virtually 100% of oxygen to be transmitted to your cornea and will often be prescribed, not as an overnight lens, but as a daily wear lens that will help with the condition, your Optometrist may decide that extended wear contact lenses that are designed to be slept in are the best option for you.
Author: John Dreyer Optometrist Bsc(Hons), MCOPTOM, DipCLP
Created: 24 Apr 2015, Last modified: 15 Feb 2024